The Role of Immune Cells Post Heart Attack
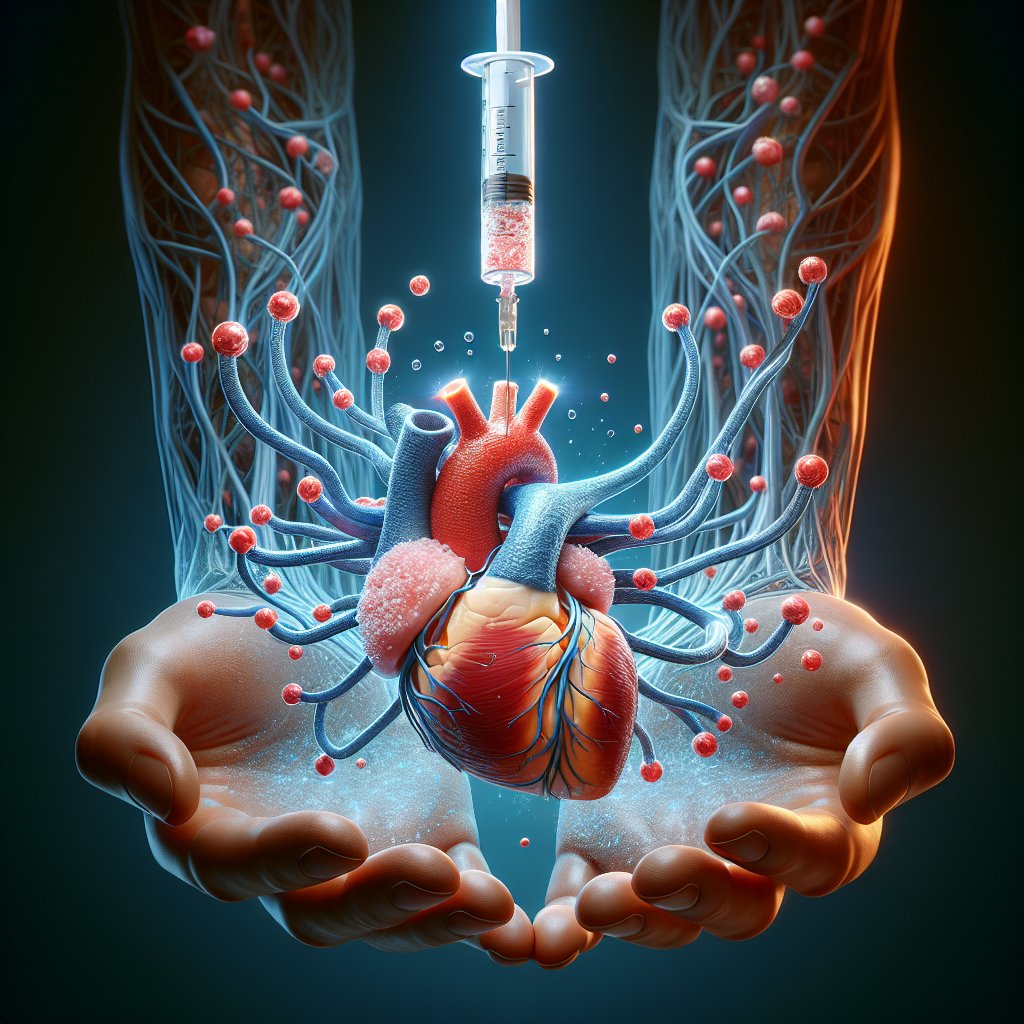
Heart attacks are no joke—especially when they come with a side of sudden cardiac death. Researchers at Massachusetts General Hospital, led by Dr. Nina Kumowski and Dr. Matthias Nahrendorf, have identified a protein that could play a crucial role in this deadly equation. It’s called Resistin-like molecule gamma (RELMy), and it’s produced by neutrophils, a type of immune cell. After a heart attack, these neutrophils flood the heart and start producing RELMy, which then attacks heart cells. This can lead to dangerous arrhythmias like ventricular tachycardia (VT) and ventricular fibrillation (VF), both of which can be fatal if not addressed immediately.
Understanding the Science Behind the Findings
So, what’s the deal with these arrhythmias? VT is when the heart beats rapidly but in a somewhat coordinated manner, while VF is more like a chaotic drum solo—uncoordinated and erratic. Both can result in sudden cardiac death. The researchers found that after a heart attack, neutrophils upregulate the gene ‘Retnlg,’ which codes for RELMy. This is not just a mouse thing; humans have a similar gene, ‘RETN,’ which is also more active in infarcted heart tissue. When they removed RELMy from neutrophils in mice, the arrhythmia burden was reduced dramatically. This suggests that targeting this protein could be a game-changer in post-heart attack treatment.
Implications for Treatment and Future Research
The implications here are significant. Currently, treatment for myocardial infarction focuses on restoring blood flow to the heart. But what if we could also target immune cells to reduce the risk of arrhythmias? Understanding the role of RELMy could lead to more targeted therapies that minimize side effects associated with broad immune suppression. The next steps involve finding a way to neutralize this pesky protein and seeing if this can reduce VT burden and infarct size—first in mice, and hopefully, eventually, in humans. It’s a promising avenue that could revolutionize how we approach cardiovascular disease.
A New Frontier in Cardiovascular Health
This research opens up a new frontier in cardiovascular health, one that doesn’t just focus on the heart but also considers the role of immune cells. If we can better understand how these cells contribute to heart disease, we can develop more effective treatments. The study was supported by various grants, including those from the Leducq Foundation and the National Institutes of Health. While some authors have disclosed affiliations with pharmaceutical companies, the research stands as a testament to the potential of targeted immune modulation in treating heart disease. It’s a reminder that sometimes the best way to protect the heart is by thinking outside the box—or in this case, the cell.